St. Mary's Saves Sick Rural Hospitals
The St. Mary’s Health Care System is expecting. The Athens-based group has acquired a hospital in Lavonia, bringing its family of hospitals to three and adding to the statewide trend of health systems buying up rural hospitals that need financial help.
The deal will move Ty Cobb Regional Medical Center, a 56-bed hospital built three years ago near Lake Hartwell, from the umbrella of Ty Cobb Healthcare System. (The Hall of Fame baseball player was from nearby Royston.) Stocked with a critical care unit, surgical suites and maternity ward, the hospital has struggled to make payments on its $47 million debt and has received help from Franklin County in the past year. As part of the deal, the hospital will be renamed St. Mary’s Sacred Heart.
Neither hospital CEO would speak about the details of the $13 million deal beyond an announcement released in late February. The acquisition took several months to move through regulatory agencies, and was finalized earlier this month.
“Our community needs and deserves quality health care, and in today’s environment, rural hospitals must be part of a larger system in order to fulfill their mission,” says Greg Hearn, Ty Cobb’s CEO.
The transition will expand the overall system’s offerings and expertise. With new regulations under the Affordable Care Act, hospitals that increase volume and attract more patients will gain the most. “This consolidation trend is happening across the country,” says Monty Veazey, president of the Georgia Alliance of Community Hospitals. “When you recruit subspecialties to your hospital, you have to keep them busy. By casting a wider net, St. Mary’s will bring in more patients.”
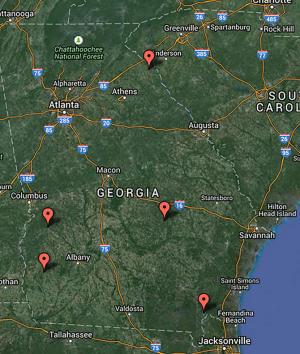
More than 50 rural hospitals have closed across the country since the beginning of 2010, according to data collected by the North Carolina Rural Health Research Program. In Georgia, five—in Hartwell, Glenwood, Folkston, Richland and Arlington—have closed since 2012, with each serving about 10,000 people, and several more are having financial problems.
“In today’s environment, it’s difficult for a small hospital to remain a standalone and be able to survive,” Veazey says. “I don’t know the details of the financials, but I would think this is a good situation for St. Mary’s, or it wouldn’t be doing it.”
State Rep. Alan Powell (R-Hartwell) who has represented Lavonia in the General Assembly for nearly 25 years, first sounded the alarm on small hospital woes about 20 years ago. As he’s become more involved in health care legislation during the past few years, Powell has watched hospitals change their business models to adapt. In fact, Ty Cobb was built three years ago because two older facilities in Hartwell and Royston were losing money and running on a dated business model. Once the facility opened in 2012, however, it faced financial problems as well.
“St. Mary’s is well run and well organized, and this will be a perfect fit for them,” Powell says. “The system will acquire the hospital for a fraction of what it would cost to build one.”
St. Mary’s acquired St. Joseph’s Hospital in Greensboro from St. Joseph’s Health System of Atlanta in 2012, renaming the 25-bed hospital as St. Mary’s Good Samaritan Hospital and turning it into the system’s “south campus.” This acquisition could make Ty Cobb the “north campus” of the three-hospital system, Powell suggests. “I think it’s a positive for the Northeast Georgia area as a whole,” he says. “It furnishes a broader picture of health care in this area.”
Founded in 1906, St. Mary’s joined Trinity Health in 2013, one of the largest Catholic health care systems in the country. With the latest changes in Medicaid reimbursements for hospitals, Trinity Health has experimented on a nationwide scale with payments and clinical quality. Here at home, St. Mary’s is expanding its offerings with hospice services, outpatient rehabilitation and stroke care.
“We are very excited about this opportunity to expand and enhance St. Mary’s mission to be a compassionate and transforming healing presence in our communities,” Don McKenna, St. Mary’s President and CEO, said during the announcement.
Before the acquisition, Ty Cobb adapted its limited resources through the Georgia Partnership for Telehealth, which connects rural hospitals in Georgia with specialists in Atlanta. The Ty Cobb arrangement, for example, used the Telestroke program to reach neurologists in Atlanta. When a patient is rushed to the emergency room in Lavonia with stroke-like symptoms, the staff can review CT, MRI and lab results with doctors in Atlanta to determine what to do next.
“If we don’t act quickly to make hospitals more viable, we’ll see more and more of them go away,” says Sherrie Williams, the partnership’s executive director. “We can’t save them all with telemedicine, but it’s a good start for them to offer services that they couldn’t before.”
To address statewide concerns, Gov. Nathan Deal established the Rural Hospital Stabilization Committee last March, approving $3 million to identify needs and potential solutions for rural hospitals. In February, he released recommendations from the committee, including a four-site pilot program that uses telemedicine to reach smaller critical access hospitals, public health departments, school clinics and local doctors. “When a rural hospital struggles, a community struggles,” Deal says.
More recently, Deal has also softened his stance against accepting federal funding for Medicaid expansion, giving a team led by Grady Memorial Hospital the go-ahead to ask the federal government for a waiver that would allow Georgia to run the program itself.
As the number of hospital mergers continues to accelerate in the state, health policy analysts are watching both positives and negatives. Consolidation may lead to better integration of health care services and better quality, but this additional leverage could also mean higher prices that are ultimately passed to the patients, says Cindy Zeldin, executive director for Georgians for a Healthy Future. “Bigger does not always mean better,” she says. “These mergers need to include consumer and community input throughout the process, so the focus can be on the patients.”
When hospital systems acquire community hospitals, managers may not be as familiar with the local community and its needs, Zeldin says. This often leads to new policies regarding uninsured patients and uncompensated care, which is typically higher in rural regions. “Will a bigger health system be able to maintain its commitment to the uninsured?” she says. “Will it be responsive and give attention to the local community?”












comments